Cardiovascular Exam For OS4
CVS Flow:
- Pulses:
- + Radial
- + Carotid
- + Peripheral
- Inspect jugular venous pressure JVP.
- Inspect Preacordium. (The area of the thorax immediately over the heart).
- Palpate the Apex – impulse and any thrills.
- Auscultate.
- Palpate Ankle / Shin for Oedema.
- Consider other signs.
- Take blood pressure.
Inspection of the nails, face, eyes and tongue:
Hands:
- Splinter haemorrhages:
- + Very common with trauma.
- + Infective endocarditis (inflam of endocardium). – 90% of this don’t have S.H.
- + Vasculitis.
- Clubbing:
- Cause is unknown.
- Thought to relate to:
- + Cyanotic congestive heart disease
- + Infective endocarditis (although late feature).
- Thought to be due to a Heart, Lung, GI & Thyroid dysfunction.
- To test for clubbing, use the Schamroth’s Window Test.
- Cyanosis:
- Low O2 saturations.
- Palmar erythema:
- A reddening of the thenar and hypothenar eminences.
- + Portal hypertension. Hypertension in the portal vein system, which is composed of the portal vein, and its branches.
- + Pregnancy.
- + Chronic liver disease.
- “Corn Beef Hands”. Progressive destruction and regeneration of the liver parenchyma (the functional tissue of an organ) leading to fibrosis (hardening).
Eyes / Face:
- Anaemia:
- Heart failure (weakness).
- A condition in which there is a deficiency of red cells or of haemoglobin in the blood, resulting in pallor (paleness) and extreme fatigue.
- Many causes. Most common = Iron-deficiency anaemia.
- + Pregnancy or childhood growth spurts are times when you need more iron than usual.
- + Heavy menstrual periods. Losing iron.
- + Poor absorption of iron from gut diseases – EG; coeliac disease and Crohn’s disease.
- + Bleeding from the intestines. You may not be aware of losing blood this way. The bleeding may be slow or intermittent, and you can pass blood out with your stools (faeces) without noticing.
- + Iron poor diet.
- Other causes:
- + Lack of Vit B12 and folic acid.
- + RBC problems like Thalassaemia.
- + Bone marrow problems and leukaemia are uncommon but can cause anaemia.
- + RA.
- + Chronic kidney disease.
- Malar Flush:
- Plum-red discolouration of the cheeks and classically associated with mitral stenosis, due to the CO2 retention w/ vasodilatory effects.
- Signs: Rosy cheeks, second degree pulmonary hypertension. PH = an increase of blood pressure in the pulmonary artery, pulmonary vein, or pulmonary capillaries, together known as the lung vasculature, leading to shortness of breath, dizziness, fainting, leg swelling and other symptoms.

- Xanthelasma:
- The appearance is of yellow flat plaques over the upper or lower eyelids.
- Hyperlipidaemia. – High cholesterol.
- Exact pathophysiology is not known.
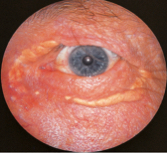
- Corneal Arcus AKA Arcus senilis:
- White, grey or blue ring in the corneal margin.
- Present at birth, but then fades, however quite common in elderly.
- Can result from hypercholesterolaemia & hyperlipidaemia
- Happens to everyone eventually.
- Can be confused with the limbus sign, which reflects calcium rather than lipid deposits (Hyperlipidaemia).

Examination of the JVP:
- Recline the patient to 45 degrees, ensure the neck is relaxed and head facing away, look between the two sternocleidomastoid heads for a pulsation. If there is a pulsation, you need to determine whether it actually is the JVP. The JVP is non-palpable, obliterated by compressing, has double waveform and is exaggerated with hepatojugular reflex.
- Once the JVP is confirmed, note its height from the sternal angle (shouldn’t be more than 3-4cm).
 Causes of a raises JVP:
Causes of a raises JVP:
- Heart failure.
- Constrictive pericarditis – Cause by a thickening of the pericardium, the membrane enclosing the heart. (JVP increases on inspiration – called Kussmaul’s sign).
- Cardiac tamponade – Type of pericardial effusion in which fluid, pus, blood, clots, or gas accumulates in the pericardium.
- Fluid overload, eg renal disease.
- Superior vena cava obstruction (no pulsation).
Examination of the peripheral pulses:
Rate, Rhythm, Volume and Character.
- Rate:
- + Normal = 60-100 BPM.
- + Bradycardia = Abnormal slow heart action = <60 BPM.
- + Tachycardia = Abnormal fast heart action = >100 BPM.
- Rhythm:
- Sinus arrhythmia (rate accelerates with inspiration and slows with exhalation).
- Can be regular or irregular.
- Can be regularly irregular or irregularly irregular = maybe Atrial Fibrillation (abnormal heart rhythm).
- Volume:
- Power of the pulse.
- High or low pulse volume.
- Character:
- Represents pulse wave form.
Changes of rate cause:
Changes of volume cause:
Peripheral pulse taking:
- Radial:
- At the wrist, lateral to the flexor carpi radialis – Medial epicondyle, bases 2nd & 3rd metacarpal bones, median n. C6 C7.
- Three fingers over one artery, assess rate, rhythm and volume.
- Count over 15 seconds and multiply by 4.
- Then palpate both radial pulses at the same time to assess volume differences – delay suggests coarctation or dissection.
- Palpate the radial and ipsilateral femoral pulse (radio-femoral delay) – delay suggestive of coarctation of the aorta.
- Brachial:
- Deep, medial to the biceps tendon, but can also be underneath.
- Use thumb to palpate with hand supporting the elbow.
- Assess the character and volume.
- Biceps = Supraglenoid tubercle (long head) coracoid process of scapula. Radial tuberosity, bicipital aponurosis of the medial forearm. Supinates the forearm. Musculocutanous n. C5-C6.
- Carotid:
- Explain to the patient the procedure.
- Never compress bilaterally.
- Patient partially reclining on the couch.
- Very gently place thumb / finger pads between the larynx and anterior border of SCM.
- Corrigan’s sign (Water-Hammer Pulse) is the medical sign which describes a pulse that is bounding and forceful, rapidly increasing and subsequently collapsing, as if it were the hitting of a water hammer that was causing the pulse. This is associated with increased stroke volume of the left ventricle and decrease in the peripheral resistance leading to the widened pulse pressure of aortic regurgitation. Listen for spread over both carotid arteries (diaphragm of stethoscope).
- Femoral:
- Patient partially reclined.
- Explain to patient and seek consent.
- Assess pulse.
- Check for radio-femoral delay.
- Popliteal:
- Can be difficult to palpate.
- If very apparent, may be due to an aneurysm.
- Try palpating the pulse with extended knee, then flexed knee.
- Dorsalis Pedis and Tibialis Post:
- Useful in detection of arterial insufficiency of lower limb.
Examining the praecordium:
- Is the portion of the body over the heart and lower chest.
- Precordial chest pain can be an indication of a variety of illnesses, including costo-chondritis and viral pericarditis.
- Observe:
- Is the patient in any obvious pain or discomfort?
- Scars.
- Chest deformity.
- Cardiac impulse.
- Pacemaker outlines.
- Palpate:
- Apex beat (5th intercostal space, mid clavicular line).
- Feel for the “heaves” – feels like an abnormally large heart beat – left ventricular hypertrophy (thickening of the left ventricular myocardium) – hypertension, strength training and cardiovascular disease.
- Feel for the “thrills” at inter costal spaces – feels like a vibration – murmur.
Auscultation:
- My – Mitral Valve and apex of heart resonates to 5 intercostal space, mid-clavicular line.
- Tits – Tricuspid valve resonates to 4/5th intercostal space, left of the sternal border
- Are – Atrial Valve resonates to the 2nd intercostal space on the right sternal border
- Perfect – Pulmonary Valve resonates to the 2nd intercostal space on the left sternal border.
What to listen for?
- S1 = Closure of the atrial valves (Mitral and Tricuspid) = “LUB” = Systole.
- S2 = Closure of the ventricular valves (Aortic and Pulmonary) = “DUB” = Diastole.
- S3 = “LUB-DUB-DUM”.
- S4 = “DA-LUB-DUB”.
Taking the blood pressure:
- Rest the patient for min of 5 mins.
- With patient seated, support the arm at level of the heart, making sure that tight clothing is not constricting the limb.
- Apply the cuff around 2 inches above the cubital fossa crease, with a 2 finger loose fit. Align the arrows of the cuff with that of the brachial artery.
- Palpate the brachial pulse and inflate the cuff until the pulse is no longer felt = rough systolic pressure. Deflate the Cuff.
- Apply the stethoscope.
- Inflate the cuff an extra 30 mmHg and listen to the brachial artery.
- Begin to deflate the cuff around 2-4 mmHg until you hear a regular tapping sound (Kortokoff sound) – systolic pressure.
- Record the pressure at which sounds disappear – diastolic pressure.
- Repeat 3 times with intervals.
- Can be either arm, but must be recored which.
- With females, be aware of the implant = a lot of pain when applying pressure.
- Over 140/90 = wait for around a minute or two, and retake.
- Pre-hypertension = 120-39/80-9
- Stage 1 = 140-59/90-99
- Stage 2 = 160-79/100-9
- Stage 3 = 180+/110+
Finally, for completion, palpate the sacrum and the shin for oedema.