Brief Examination of the Lymph Nodes
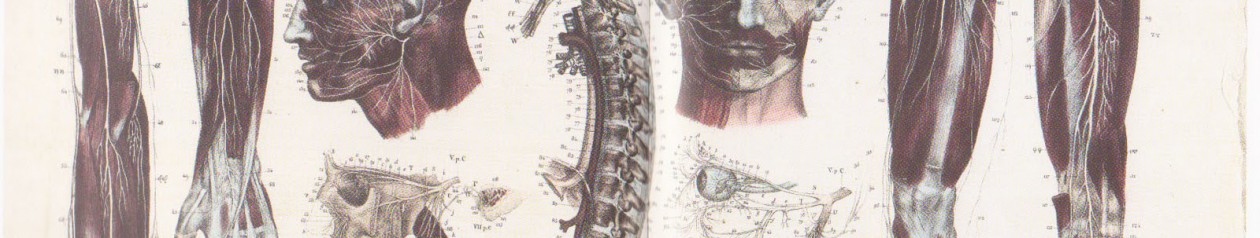
The lymphatic system is a series of vessels throughout the body that drain fluid from tissues. Bacteria and other microbes are picked up in the lymphatic fluid and trapped inside the lymph nodes, where they can be attacked and destroyed by white blood cells. Common problems of the lymphatic system include Glandular Fever, Hodgkin’s disease, Oedema and tonsillitis.
Sequence: Inspect the patient for a visible lymphadenopathy (any disease of the lymph nodes). Afterwards, palpate the patient one side at a time, whilst comparing with the nodules on the contralateral side.
Assessment:
- Site.
- Size.
- Consistency.
- Tenderness.
One major side is on the left supraclavicular fossa (the seat of the Devil) – Virchow’s Node – Linked to abdomen cancer. Known as Troisier’s sign. Suspect this if the node is hard and enlarged above the average (0.5cm) and the max being 2.0cm. Fixation of lymph nodes also points towards malignancy.  Consistency – Normal nodes feel soft. They can also feel tender (acute viral or bacterial infection). It is important to know that sometimes it is natural to have naturally large lymph nodes in some individuals. Proceed with caution anyway.
Consistency – Normal nodes feel soft. They can also feel tender (acute viral or bacterial infection). It is important to know that sometimes it is natural to have naturally large lymph nodes in some individuals. Proceed with caution anyway. 
























 find my feet! 😀
find my feet! 😀