Full Cranial Nerve Examination For OS4.
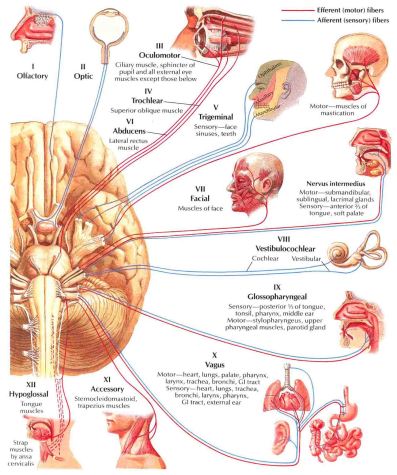
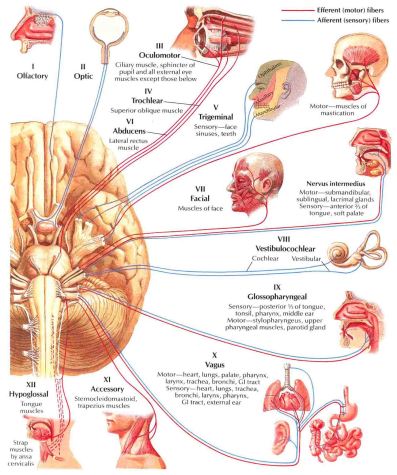
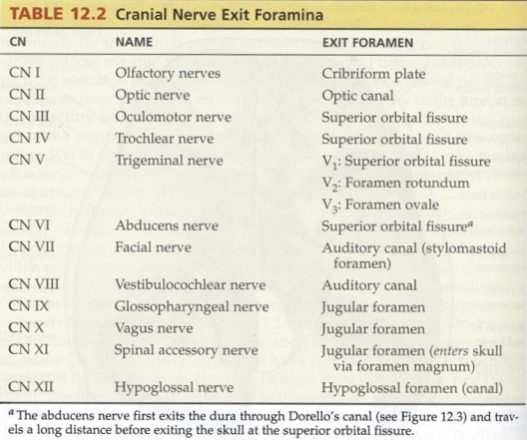
The 12 Cranial Nerves are:
- I Olfactory.
- II Optic.
- III Oculomotor.
- IV Trochlear.
- V Trigeminal.
- VI Abducent.
- VII Facial.
- VIII Vestibulocochlear.
- IX Glossopharyngeal.
- X Vagus.
- XI Accessory.
- XII Hypoglossal.

- The Cranial Nerves’ Song!! – https://www.youtube.com/watch?v=IBuPzn_8UTc
Bear in mind that this is a rude way to remember the 12 cranial nerves, but please don’t be offended, its just for memory purposes. There are plenty of ‘clean’ options too on the internet. I use:
Oh, Oh, Oh, To, Touch, And, Feel, Virgin, Girl’s, Vaginas, Ahh!, Heaven.
Classification of Cranial Nerve Functions:
- Sensory: Contain only afferent fibres:
- I Olfactory.
- II Optic.
- VIII Vestibulocochlear.
- Motor: Contains only efferent fibres:
- III Oculomotor.
- IV Trochlear.
- VI Abducent.
- XI Accessory.
- XII Hypoglossal.
- Mixed nerves: Contains both efferent and afferent fibres:
- V Trigeminal.
- VII Facial.
- XI Glossopharyngeal.
- X Vagus.
Mnemonic: Again, apologies for being rude, but there are ‘clean’ alternatives on the internet.
S= Sensory, M= Motor, B = Both.
- Skinny Sluts Make,
- Money But My,
- Brother Says Big,
- Bitches Make More.
- I Olfactory, II Optic, III Oculomotor,
- IV Trochlear, V Trigeminal, VI Abducent,
- VII Facial, VIII Vestibulocochlear, IX Glossopharyngeal,
- X Vagus, VI Accessory, XII Hypoglossal.
CN 1 – Olfactory Nerve:
- Olfactory bulb origin.
- Cribiform plate.
- Sensory.
- Vulnerable to:
- + Fractures.
- + Tumours.
- + Parkinson’s Disease. Progressive nervous system degeneration of the basal ganglia and a deficiency of the neurotransmitter dopamine. Marked by tremor, muscular rigidity.
- + Huntington’s Disease. A hereditary disease. Degeneration of brain cells and causing chorea (Kaw-rea) and progressive dementia (memory disorders, personality changes, and impaired reasoning).
- Disruption leads to loss of smell, full or partial.
- Examination:
- Patient closes one nostril and both eyes.
- Present coffee to identify.
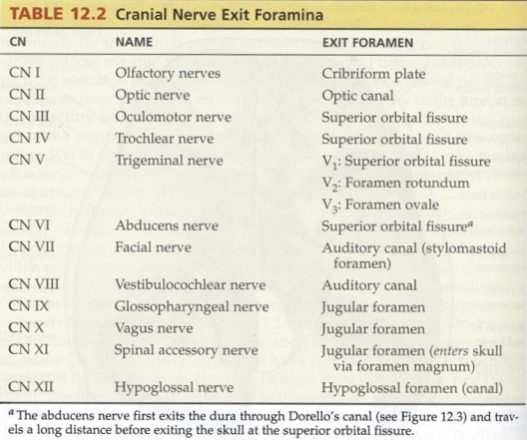
CN 2 – Optic Nerve:
- Sensory.
- Visual pathway from retina, chiasma, optic tracts leading to the visual cortex.
- Disruption –> visual disturbances, visual agnosia (can see but can’t interpret the information), disturbances of perception and hallucinations.
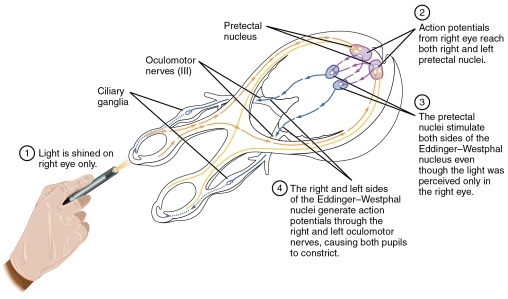
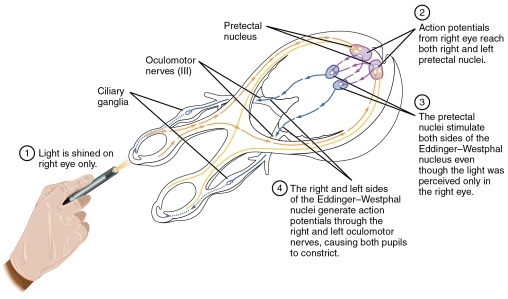
- How the pupils respond to light:
- Direct and consensual response:
- The direct response:
- + Meaning constriction of the illuminated pupil.
- + The direct response is impaired in lesions of the ipsilateral optic nerve, the pretectal area (midbrain structure), the ipsilateral parasympathetics traveling in CN III, or the pupillary constrictor muscle of the iris.
- The consensual response:
- + Meaning constriction of the opposite pupil.
- + The consensual response is impaired in lesions of the contralateral optic nerve, the pretectal area, the ipsilateral parasympathetics traveling in CN III, or the pupillary constrictor muscle.
- How it works:
- Information enters via CN2 – Optic & activates CN3 – Oculomotor.
- This is a consensual (both eyes are involved) parasympathetic reflex.
- If only the eye being tested constricts, then there is damage to the crossing fibres (damage in the midbrain).
- Examination:
- Vision chart.
- Colour blind test.
- Visual reflexes:
- + Patient covers one eye, shine pen torch into one eye for approx 1 second. – Pupil constriction.
- Accommodation:
- + Testing for the pupillary response. Normally the pupils constrict whilst fixating on an object being moved from far to near the eyes.
- + Tell the patient to focus on the furthest point of the room, and to focus when adding the pen into their vision.
- Accommodation is impaired in lesions of the ipsilateral optic nerve, the ipsilateral parasympathetics traveling in CN III, or the pupillary constrictor muscle, or in bilateral lesions of the pathways from the optic tracts to the visual cortex.
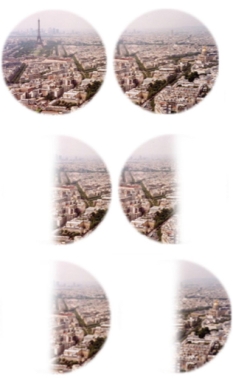
- Visual field test:
- + Ask patient to keep their eyes looking towards your nose.
- + In all four quadrants, wiggle your fingers and ask the patient to identify if they see them.
- Common field defects include:
- 1 = Bitemporal Heminanopia: Lesion at the optic chiasm (Pituitary tumour).
- 2= Homonymous Heminanopia: Lesion posterior to the optic chiasm (Posterior cerebral artery territory infarction).
- 3= Blindness in one eye: Lesion in the eye, retina or the optic nerve.
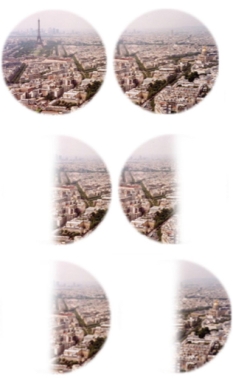

- Expansion of the blind spot – central scotoma.
- Central scotoma is an area of depressed vision that corresponds with the point of fixation and interferes with central vision. It suggests a lesion between the optic nerve head and the chiasm.
- + Multiple sclerosis – which may cause unilateral or asymmetrical bilateral scotoma
- + Nutritional causes – which may be due to, e.g. alcohol or tobacco amblyopia, B12 deficiency
- + Vascular lesions – which may cause unilateral scotoma
- + Gliomas of the optic nerve – this may cause unilateral scotoma
- + Simple glaucoma – which may initially cause an off-centre scotoma

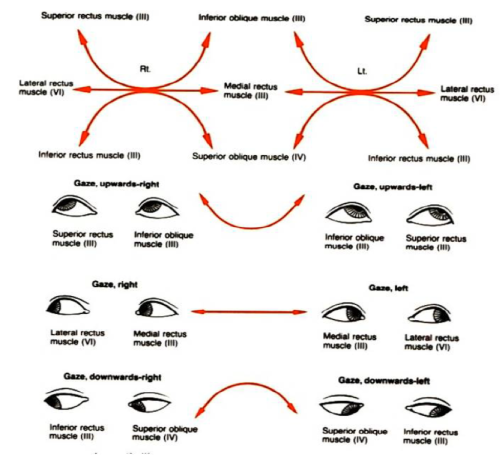
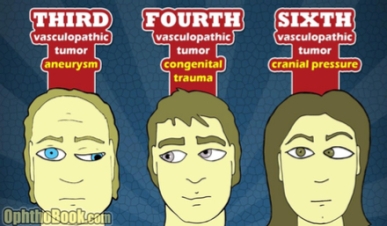
CN III – Oculomotor, CN IV – Trochlear & CN VI – Abducent:
- All involved in movements of the eye.
- + Oculomotor: Motor, Oculomotor nucleus, Edinger-Westphal nucleus (both in the midbrain) divides into superior and inferior, through the superior orbital fissure (SOF) and into the orbital cavity. All other extraocular muscles, also carries parasympathetic (constrictor) fibres to pupil, and fibres to levator palpebrae superioris.
- + Trochlear: Motor, Dorsal Midbrain, SOF, orbital cavity. Supplies superior oblique muscle
- + Abducent: Motor, Lower Pons, SOF, orbital cavity. Supplies lateral rectus muscle
- For the full anatomy, see the link for a short powerpoint: http://www.slideshare.net/farhan_aq91/cranial-nerve-iii-iv-and-vi
- Examination:
- The ‘H’ Test:
- + Ask the patient to keep their head in a straight position, whilst using a (preferably red tipped) pen and draw an H shape with their eyes following.
- + Ask the patient to report any Diplopia (double vision), if so, at what point. Also keep an eye out for nystagmus (involuntary eye shaking).
- http://www.nhs.uk/Conditions/Double-vision/Pages/Causes.aspx
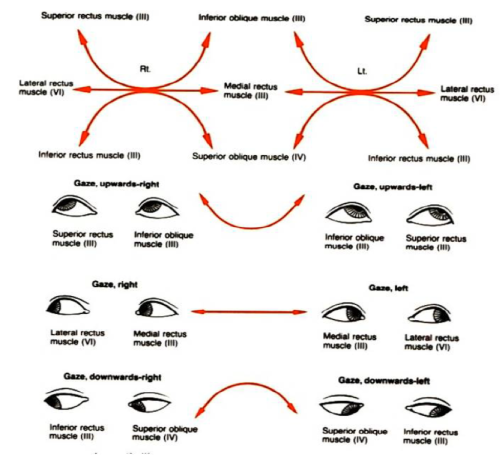
Eye Movements:
- Look at eyes in a relaxed state.
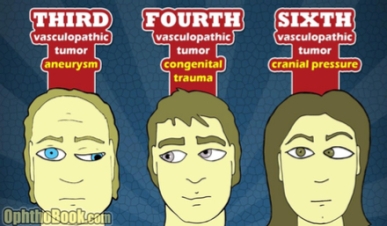
- 3rd nerve palsy:
- + Eye often down and out.
- 6th nerve palsy:
- + Osten eyes convergent (unchallenged medial rectus).
- Look at the pupils. – Dilation – bilateral or unilateral?
- Look for drooping of the eye lid = Ptosis.
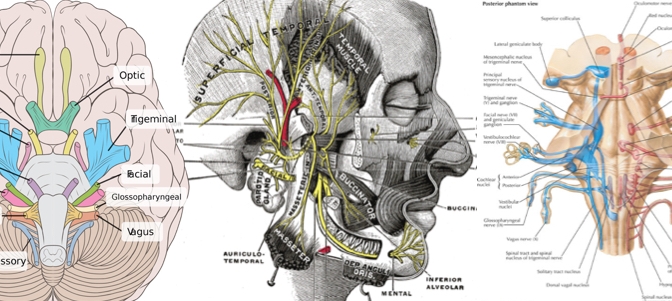
CN V – Trigeminal Nerve:
- Both sensory and motor.
- Pons, Medulla and Midbrain origin.
- Exits:
- + V1 = SOF.
- + V2 = Rotundum.
- + V3= Ovale.
- Sensory = face.
- + 3 branches = ophthalmic, maxillary and mandibular.
- Motor = mastication = masseter and temporalis.
- Examination:
- Sensory = cotton wool.
- + Jaw line.
- + Cheeks.
- + Forehead.
- The corneal reflex could also be examined as the sensory supply to the cornea is from this nerve.
- Do this by lightly touching the cornea with the cotton wool. This should cause the patient to shut their eyelids.
- Motor = Muscle testing.
- Ask the patient to clench their teeth, whilst feeling the temporals and masseter muscles.
- Ask the patient to open their mouth against practitioner resistance.
- Finally, perform the jaw jerk on the patient by placing your left index finger on their chin and striking it with a tendon hammer. This should cause slight protrusion of the jaw.
CN 6 – Abducent Nerve:
- Tested with CN III & CN IV.
- Dysfunction of ipsilateral rectus muscle leads to lateral gaze palsy.
CN 7 – Facial Nerve:
- Motor and Sensory and Para Sympathetic.
- Pons. Exits Internal Auditory Meatus & Stylomastoid foramen.
- Motor:
- + Muscles of facial expression.
- Sensory:
- + Anterior 2/3rd’s of tongue.
- Para Symp:
- + Supply to lacrimal, submandibular and sub lingual glands.
- Dysfunction:
- + Bell’s palsy.
- +/- Ageusia – Inability to taste.
- +/- Hypogeusia – Reduced ability to taste.
- Examination:
- Facial expressions.
- + Frown.
- + Raise eye brows.
- + Smile – teeth showing.
- + Blow cheeks out.
- + Keeps eyes closed against resistance.
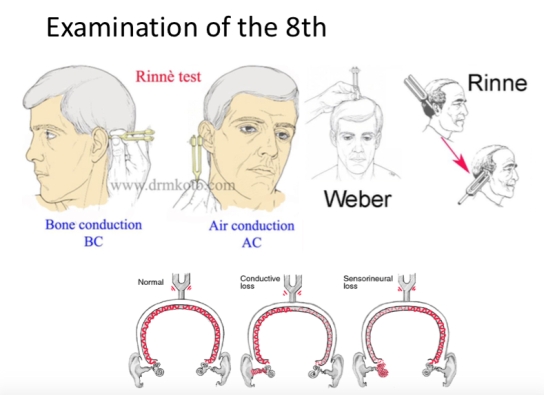
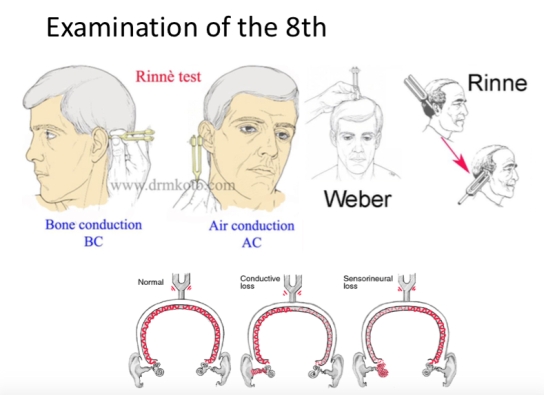
CN 8 – Vestibulocochlear:
- Sensory.
- Pons and Medula Oblongata. Exits internal acoustic meatus of the temporal bone.
- Hearing and equilibrium
- Provides innervation to the hearing apparatus of the ear and can be used to differentiate conductive and sensori-neural hearing loss using the Rinne and Weber tests.
- Conducts two special senses:
- Hearing (audition) and balance (vestibular). The receptor cells for these special senses are located in the membranous labyrinth which is embedded in the petrous part of the temporal bone.
- Positional vertigo is the most common problem, although tinnitus, hearing loss, and deafness may also occur following damage. Positional vertigo occurs, usually for about 30 seconds, with sudden changes in position, usually from lying to sitting or from sitting to standing.
-
- Examination:
- To carry out the Rinne test: Place a sounding tuning fork on the patient’s mastoid process and then next to their ear and ask which is louder. A normal patient will find the second position louder.
- To carry out the Weber’s test: Place the tuning fork base down in the centre of the patient’s forehead and ask if it is louder in either ear. Normally it should be heard equally in both ears.



CN 9 – Glossopharyngeal:
- Both motor and sensory and para sympathetic.
- Medulla oblongata, exits through the jugular foreman.
- Sensory: taste from posterior 1/3rd of the tongue, larynx, carotid sinus and body.
- Motor: pharyngeal muscle.
- Para symp: Salivary glands.
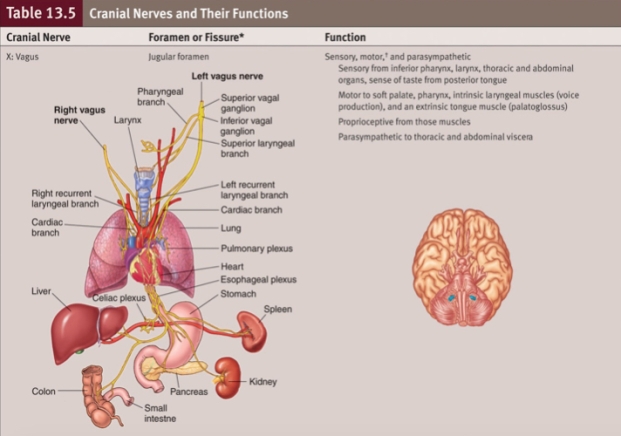
CN X – Vagus:
- Both motor and sensory.
- From the brain stem, through the jugular foreman to the viscera.
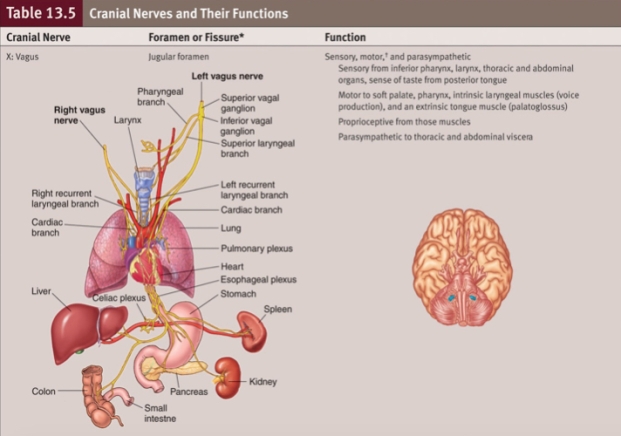
- Examination of CN IX & X:
- The Glossopharyngeal nerve: Provides sensory supply to the palate. It can be tested with the gag reflex or by touching the arches of the pharynx.
- The Vagus nerve (CN X): provides motor supply to the pharynx. Asking the patient to speak gives a good indication to the efficacy of the muscles. The uvula should be observed before and during the patient saying “aah”. Check that it lies centrally and does not deviate on movement.
- Dysfunction: Glossopharyngeal nerve & Vagus nerve:
- Damage results usually from surgery, cancer, aortic arch aneurysms.
- Dysfunction:
- Dysphagia (difficulty swallowing) and dysarthria (difficulty talking) are caused by injury to the nuclei of the glossopharyngeal and vagus nerves.
- Aphonia (inability to speak through disease of or damage to the larynx or mouth) or weak/hoarse voice are caused by injury to the vagus nerve.
CN XI – The Accessory Nerve:
- Motor.
- Medulla oblongata, jugular foramen and foramen magnum.
- SCM and Trapezius muscles, pharynx and soft palate.
- Spinal part prone to injury as it travels in the posterior lateral portion of the cervical spine.
- Examination:
- Cranial part – Testing the SCM. – resisted sidebending and rotation.
- Spinal part – Testing the trapezius. – resisted shoulder shrug.
CN XII – Hypoglossal Nerve:
- Motor.
- Origin is the medulla oblongata, exiting out of the hypoglossal canal.
-
Supplies all the intrinsic muscles and all extrinsic (except one) of the tongue, and the Styloglossus, Geniglossus, Hyoglossus.
- Examination:
- Observe the tongue for any signs of wasting or fasciculations.
- Ask the patient to stick their tongue out and move left, right, up, down. If the tongue deviates (on protrusion) or can’t complete to either side, it suggests a weakening of the muscles on that side.
Thank you for reading! I hope you found this helpful! If you have anything to add, please let me know!
Like, Share, Comment, Follow.
 Consistency – Normal nodes feel soft. They can also feel tender (acute viral or bacterial infection). It is important to know that sometimes it is natural to have naturally large lymph nodes in some individuals. Proceed with caution anyway.
Consistency – Normal nodes feel soft. They can also feel tender (acute viral or bacterial infection). It is important to know that sometimes it is natural to have naturally large lymph nodes in some individuals. Proceed with caution anyway.